Diastolic Function & Diastolic Dysfunction
Definition
Diastolic function is defined as/describes the filling of the heart during diastole. The left ventricle is filled with blood initially by a pressure gradient between the left atrium (LA) and the left ventricle (LV). Especially ventricles of young healthy individuals also create suction in the very early phase of filling due to a rapid expansion of the LV. In between passive and active filling of the left ventricle there is a period of time where only little filling occurs, the so-called diastasis. Therefore diastolic dysfunction is understood as impaired left ventricular relaxation with increased stiffness of the LV and elevated filling pressures.
Cardiac Filling MasterClass
Sign up now for our course Cardiac Filling MasterClass and get FREE LECTURES.
Clinical context & background
Possible causes of diastolic dysfunction are various such as structural heart diseases (hypertrophy, constriction, fibrosis) or functional heart disease (ischemia). Diastole is affected by a lot of factors such as heart rate, ventricular function and compliance, preload, atrial systolic function, heart rhythm and atrioventricular valve function. The prevalence of diastolic dysfunction in over 25% of the adult population over 40 years of age!
Echocardiography should be used as a tool in patients showing signs or symptoms of heart failure, e.g. dyspnea to evaluate if there is diastolic dysfunction present.
Variables
There are various variables to assess diastolic function using corresponding pathological cut off values:
- Mitral E/A ratio - cut off value: ≤ 0.8 & > 2
- Peak E velocity - cut off value: > 50 cm/sec
- Deceleration time (DT) - cut off value: 140 - 240 msec
- e´ - cut off values: septal < 7cm/sec, lateral < 10cm/sec
- E/e´ ratio - cut off value: average > 14 (septal >15 , lateral >13)
- Left atrial (LA) maximum volume index - cut off value: 34mL/m2
- Peak tricuspid regurgitation (TR) velocity - cut off value: > 2.8m/sec
- Isovolumic relaxation time (IVRT) - cut off value: ≤ 70 mm/sec - >100 mm/sec
- pulmonary venous S/D ratio - cut off value:
- Ar - A duration - cut off value: >30 msec
Grading
Note: A grading of diastolic dysfunction is only relevant in patients with reduced EF or structural heart disease, because it may change treatment decisions.
- Grade I diastolic dysfunction, impaired relaxation: First stage of diastolic dysfunction. Decreased suction of the LV.
- Grade II diastolic dysfunction, pseudonormalization: Increased stiffness of the LV, elevated LAP.
- Grade III, restrictive filling (reversible): High LAP, noncompliant LV. May be reversible with reduction of preload (e.g. diuretics).
- Grade IV, restrictive filling (irreversible): As stage III with no benefit from a reduction of preload.
Patient evaluation
Before evaluating diastolic function it is important to differentiate between patients with normal left ventricular EF and reduced left ventricular EF or structural heart disease since the focus is a different one (existence of diastolic dysfunction vs. estimation of filling pressures). However, in both cases you need to obtain the average E/e’, LA maximum volume index and peak TR velocity. In patients with normal EF you need to additionally evaluate either septal or lateral e’, while in patients with reduced EF you need to evaluate peak E wave velocity and E/A ratio.
Since you need the peak E wave velocity for E/e’ it is a good idea to start with the mitral inflow pattern, although the pattern itself is only important in patients with reduced EF. The peak of the passive filling of the LV (peak E wave) and the active contraction of the left atrium in atrial systole (peak A wave) should be assessed, and an E/A ratio should be calculated. The next step is to assess septal and lateral e’ and calculate an average E/e’ to get all specific parameters of diastolic function, since the LA maximum volume index and peak TR velocity are usually part of every echocardiographic exam.
More on how to obtain those measurements here: How to assess diastolic function.

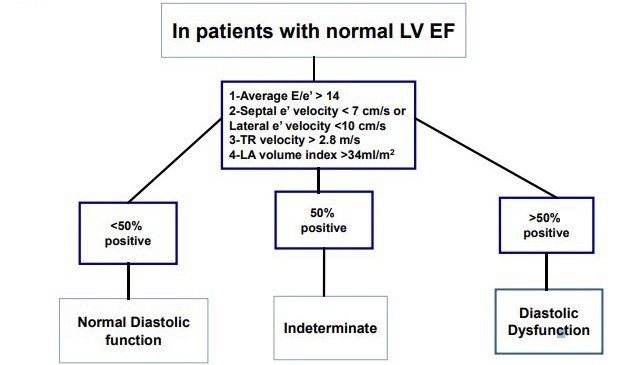
Evaluation in patients with preserved EF
In patients with preserved ejection fraction (EF) according to the current guidelines one should evaluate four variables to assess diastolic dysfunction: e´, E/e´ ratio, LA maximum volume index and peak TR velocity. If three or more of the parameters are abnormal there is diastolic dysfunction present. In the case of 2 abnormal and 2 normal parameters diastolic function cannot be assessed and if three ore more are non-pathological normal diastolic function is present.
See how the you can approach the grading of diastolic dysfunction in this chapter of our ebook.
See how the you can approach the grading of diastolic dysfunction in this chapter of our ebook.
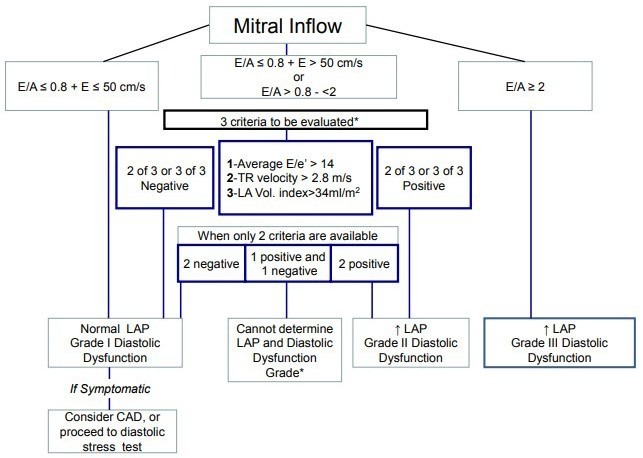
In patients with reduced left ventricular EF an E/A ratio of ≤ 0,8 and with a peak E velocity of 50 cm/sec or lower denotes normal filling pressures, equals grade I of diastolic dysfunction. If E/A ratio is > 2 means that left atrial filling pressures are elevated and and is classified as diastolic dysfunction grade III is present.
An E/A ratio of ≤ 0.8 with a peak E velocity of over 50 cm/sec or an E/A ratio > 0.8 but
Pulmonary vein peak systolic to peak diastolic velocity should be used if one of the other variables is not available in patients with reduced left ventricular ejection fraction. Note that normal pulmonary flow consists of a systolic and a diastolic component and a very brief flow reversal (negative wave) during atrial systole.
If you want to get further insights into current diastolic function & dysfunction guidelines you can watch our free webinar here.
Specific situations
Diastolic stress testing:
Indication: If resting echo does not explain the symptoms of heart failure or dyspnea especially with exertion. It is considered positive if all three criterias apply:
- average E/e´ > 14 or septal E/e´ ratio > 15 with exercise
- peak TR velocity > 2.8 m/sec with exercise
- septal e´ velocity is < 7 cm/s or lateral is < 10 cm/s at baseline
Pitfalls & Tipps
L-Wave: Under normal conditions during diastasis there is no flow from the left atrium to the LV. If flow occurs (usually during bradycardia) this wave is called an L-Wave and denotes elevated filling pressures.
Supernormal filling: In young, fit and healthy individuals you can see a very tall E-wave, a normal DT, a very small A-wave and an E/A ratio >2 which looks like a restrictive filling pattern. This is due to a very strong suction of the LV during diastole.
Be aware that suboptimal Doppler signals can lead to misinterpretation. You should not interpret such a signal.
Be aware that one normal parameter (e.g. a normal sized left atrium) does not automatically indicate normal diastolic function and exclude diastolic dysfunction.
Note IVRT is prolonged in impaired relaxation, gets shorter with left atrial pressure (LAP) elevation. Be aware that IVRT becomes longer when people get older and influenced by heart rate and systolic function.
Be aware that in young healthy individuals the S/D ratio of pulmonary venous flow is often below 1.
Be aware that you can not measure E/A ratio in the presence of atrial fibrillation (AFIB), significant mitral regurgitation, significant mitral annular calcification, left bundle branch block (LBBB), paced rhythm or mitral stenosis. In patients with AFIB you can use E/e´ ratio and IVRT which is shortened.
Be aware that when you measure E/e´ ratio the variables are measured at different times in the cardiac cycle. It is age dependent, preload dependent and it varies when left ventricular systolic function changes. You should not measure e´ when a prosthetic valve, an annuloplasty or mitral annular calcification is present. Left atrial (LA) maximum volume index gives diagnostic and prognostic information. There is still no targeted therapy for patients with diastolic dysfunction.
Left atrial (LA) maximum volume index gives diagnostic and prognostic information. Note that an increased LA volume index can also be found physiologically in well-trained athletes with bradycardia.
There is still no targeted therapy for patients with diastolic dysfunction.
See this chapter for more details: How to assess diastolic function
Clinical assessment of left ventricular diastolic function.
Derek G Gibson and Darrel P Francis; Heart. 2003
Understanding the Epidemic of Heart Failure: Past, Present, and Future
Shannon M. Dunlay et al., Curr Heart Fail Rep. 2014
Prevalence of left ventricular diastolic dysfunction in a general population.
Kuznetsova T et al., Circ Heart Fail. 2009
Assessment and impact of diastolic function by echocardiography in elderly patients
Clementina Dugo et al., J Geriatr Cardiol. 2016
Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging
Sherif F. Nagueh et al., J Am Soc Echocardiogr 2016 (PDF)

