9. Assessment of intima media thickness (IMT)
9.1 Why should the intima media thickness be measured with ultrasound?
One of the main indications for a carotid ultrasound scan is the assessment of cerebrovascular risk. The presence of atherosclerotic plaques clearly point to an increased risk (not only for stroke, but also for coronary artery disease and peripheral vascular disease). While it is debatable if the intima media thickness should routinely be used for risk assessment there is strong evidence that the intima media thickness (if measured correctly) provides valuable information with respect to cardiovascular risk. Numerous clinical and epidemiologic studies demonstrated an association with coronary artery disease, stroke and peripheral vascular disease and intima media thickness. Therefore, measurements of intima media thickness should be part of every extra-cranial ultrasound exam. Especially, since measurements of the intima media complex are easy to be obtained with carotid ultrasound.
Note: An increase in the intima media thickness can also be found in non-atherosclerotic disease (such as vasculitis or as a response to hypertension)
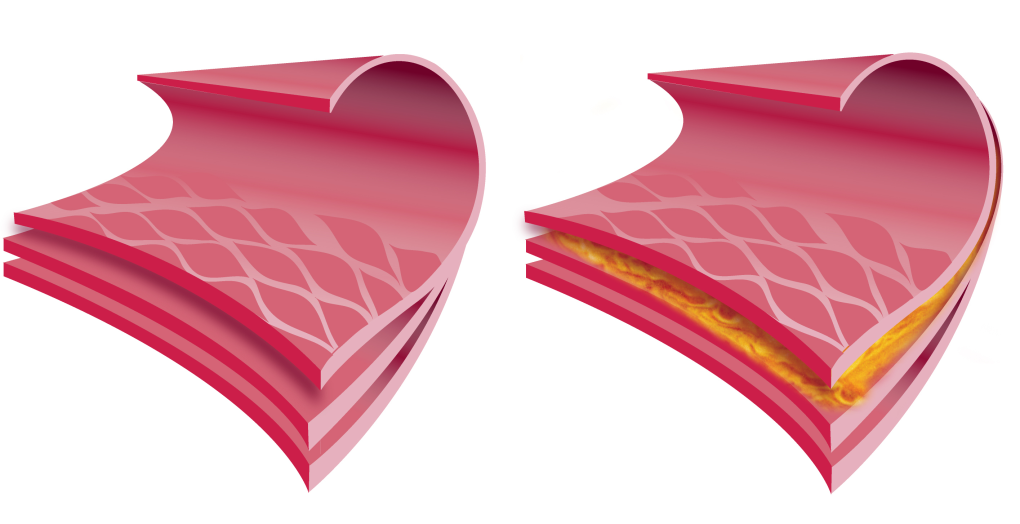
 Intima media. The intima media complex is the layer of the arter, which is mostly affected in the process of atherosclerosis
Intima media. The intima media complex is the layer of the arter, which is mostly affected in the process of atherosclerosis
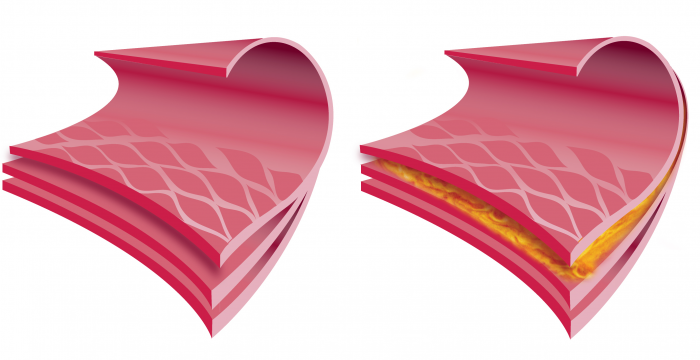
9.2 What are the components of the arterial wall.
The arterial wall consists of 3 layers:
- Tunica intima
- Tunica media
- Tunica externa
While the wall of veins also have a tunica intima, tunica media and tunica externa it greatly differs from the arterial wall as it is much thinner and lacks the internal and external elastic membrane. Because veins do not have to withstand high pulsatile pressures they only have a thin layer of smooth muscles.
 IM Histology. Layers of the artery wall: The tunica intima is the inner layer. It consists to the basement membrane, the stratum subendothelium and the internal elastic membrane. The tunica media consists to smooth muscle cells and collagen fibers. The tunica externa consists of the external elastic membrane, the serosa, nerves and blood vessels (vasa vasorum)
IM Histology. Layers of the artery wall: The tunica intima is the inner layer. It consists to the basement membrane, the stratum subendothelium and the internal elastic membrane. The tunica media consists to smooth muscle cells and collagen fibers. The tunica externa consists of the external elastic membrane, the serosa, nerves and blood vessels (vasa vasorum)
9.3 How should I image and measure the intima media with ultrasound?
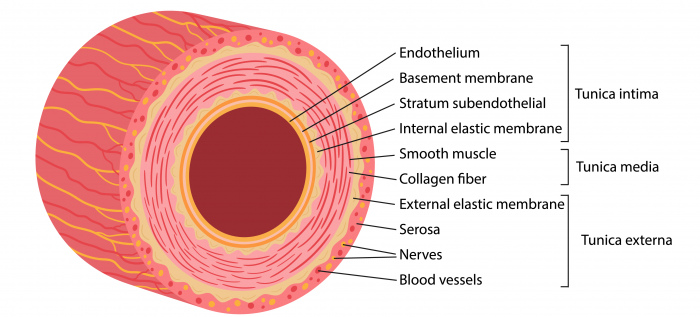
Imaging and measuring the intima media thickness Use high resolution images (zoom/ optimal depth, high scanline density) Optimize the angel of insonation (90° to the vessel wall) Measure the posterior wall (far field) or both (average the anterior and posterior wall) i.e. for research purposes Measure at least 5mm proximal to the distal end of the CCA Measure at a segment which is free of atherosclerotic plaque Measure in a straight segment (at least 10mm long) Also observe the echogenictiy of the IMT (increase in the echogenicity of the media)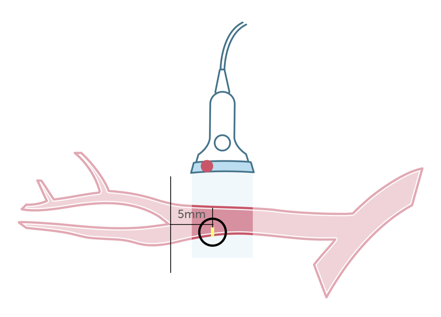 IMT Where IMT. This illustration shows the region where the measurements of the intima media thickness should be performed. The measurement should be obtained 5mm from the bifurcation. Ideally both the posterior and the anterior wall should be measured
IMT Where IMT. This illustration shows the region where the measurements of the intima media thickness should be performed. The measurement should be obtained 5mm from the bifurcation. Ideally both the posterior and the anterior wall should be measured
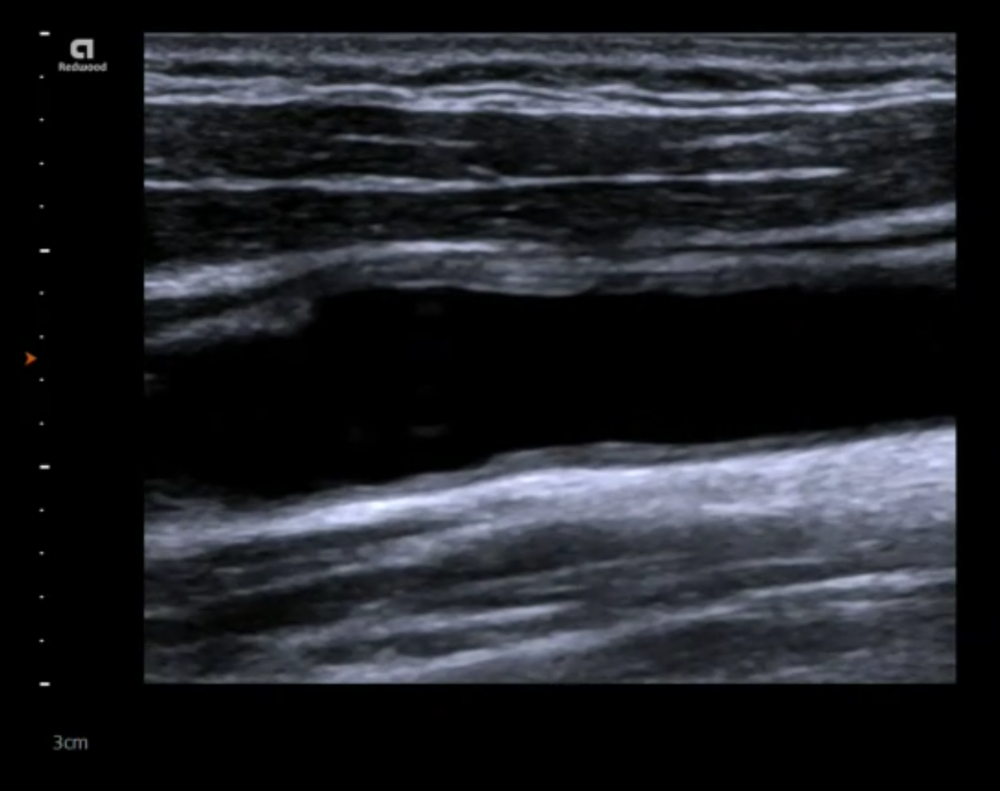
9.4 How can I recognize the intima media layer appear on ultrasound?
The intima, media and tunica externa layers are easy to discern with ultrasound as they have different echogenicities. The intima and the externa / adventia is usually bright (highly reflective), while the media is less echogenic. Be aware though that the echogencity, especially of the media can increase in the presence of fatty infiltration, plaque formation and thickening.
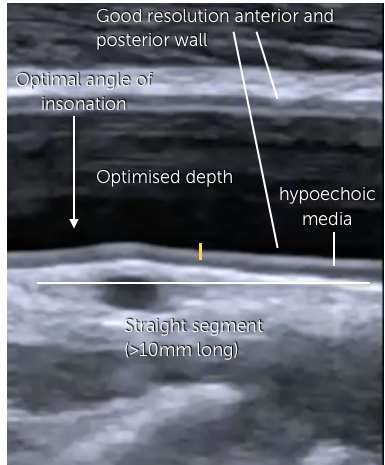 IMT Image explain Ultrasound of the common carotid artery: Image optimization for intima media thickness measurements. The intima media should clearly be visible
IMT Image explain Ultrasound of the common carotid artery: Image optimization for intima media thickness measurements. The intima media should clearly be visible
9.5 What is the normal intima media thickness?
An upper limit of 0.9 mm has been proposed as a cut off value that denotes an increased cardiovascular risk. However, the intima media thickness increases with age and also varies between males and females. It has therefore been proposed to use a higher cut off value for elderly patients. There have also been attempts to convert intima media thickness into “vascular age”
IMT normal values
Men P25 P50 P75 <30 0.42 0.44 0.49 31-40 0.44 0.47 0.57 41-50 0.50 0.55 0.61 >50 0.53 0.61 0.70 Women P25 P50 P75 <30 0.30 0.44 0.47 31-40 0.44 0.47 0.51 41-50 0.46 0.51 0.57 >50 0.52 0.59 0.64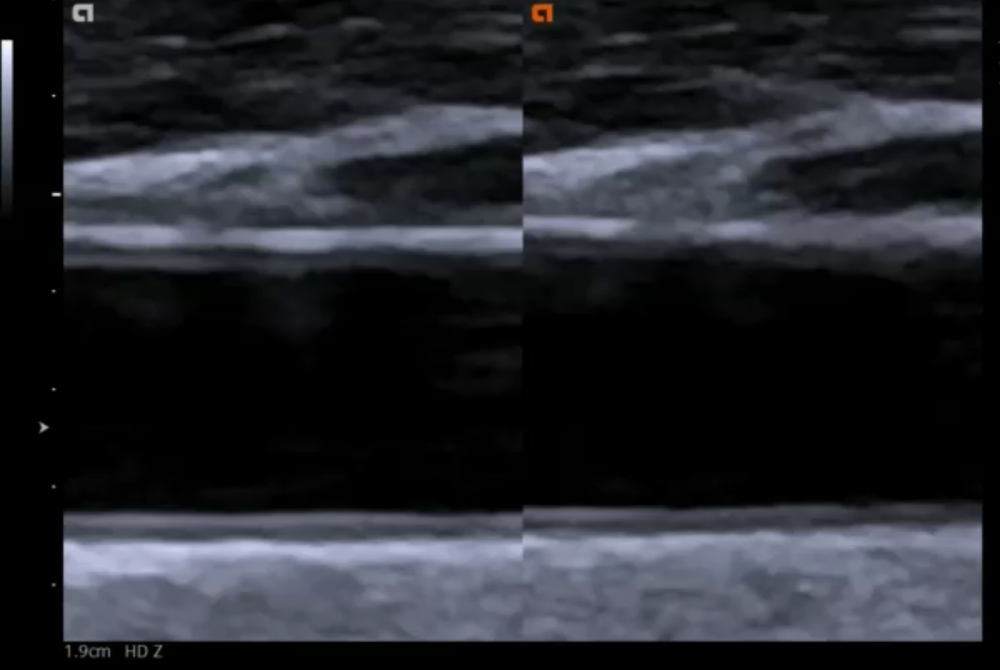 IMT normal. Ultrasound of the common carotid artery: Normal intima media thickness (0.4mm) in a young healthy individual. Note that the intima is echogenic while the media is hypogenic
IMT normal. Ultrasound of the common carotid artery: Normal intima media thickness (0.4mm) in a young healthy individual. Note that the intima is echogenic while the media is hypogenic
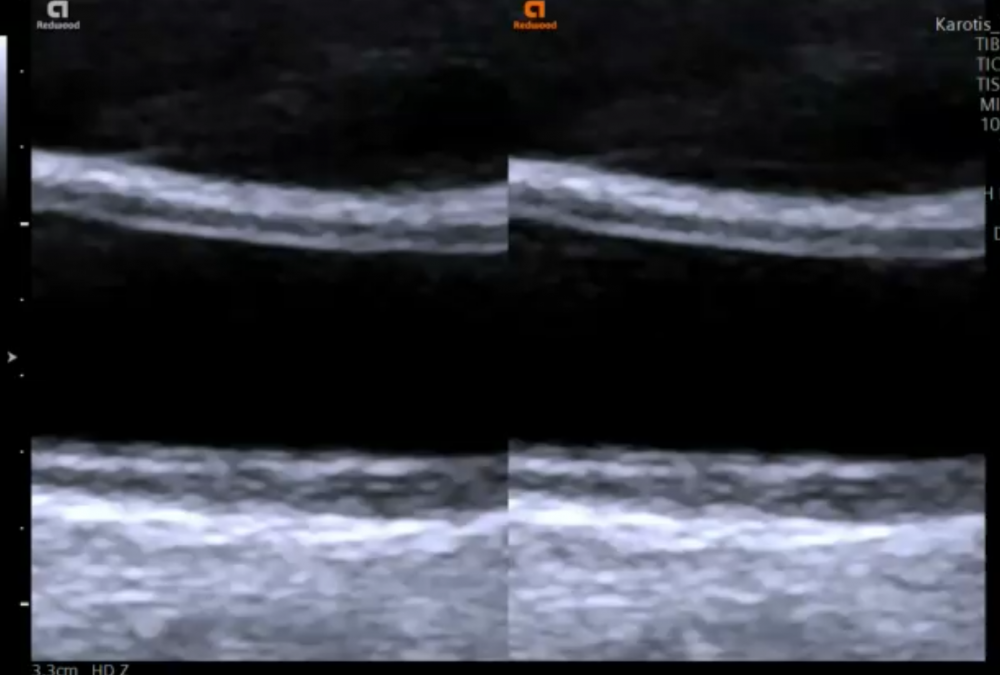 IMT thickened. Ultrasound of the common carotid artery: Increased intima media thickness (1.3mm) in an elderly patient with hypertension
IMT thickened. Ultrasound of the common carotid artery: Increased intima media thickness (1.3mm) in an elderly patient with hypertension
9.6 What are the limitations of intima media measurements?
The intima media is measured in the common carotid artery where atherosclerosis is less pronounced than in other parts of the vessel (such as the bifurcation or the carotid bulb). Measurements are in the millimeter range, so small motions of the trackball will already result in a rather large difference (measurement error). Finally, It is important to optimize the angel of insonation to get a good delineation of the intima media thickness.
9.7 How does atherosclerosis affect the intima media and lead to plaque formation?
Atherosclerosis is the build up of plaque and the hardening of arteries. In a way atherosclerosis can be considered “the process of aging” of the arteries. Many factors contribute to this process (i.e. hypertension, smoking, diabetes, kidney disease). Risk factors accelerate the process of atherosclerosis. In the initial phases you will see an increase in the intima media thickness followed by plaque formation. Ultimately these plaques can lead to obstruction (stenosis) or even occlusion of the artery.
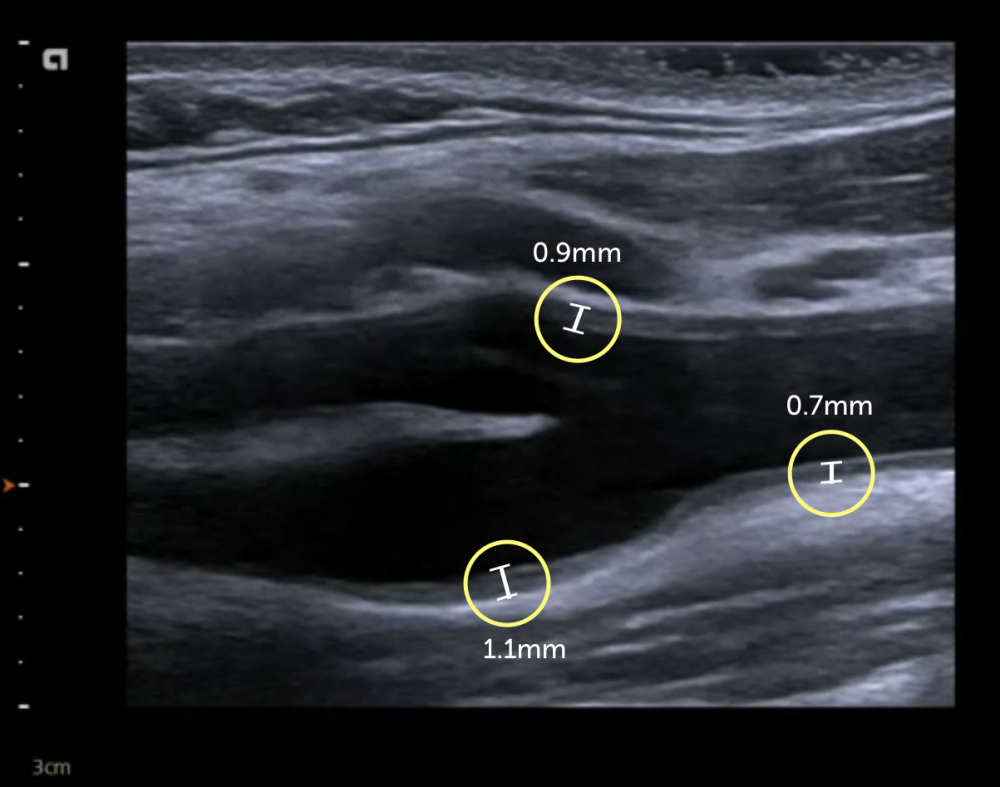 ariation IMT. Measurements of the intima media thickness in different regions of the carotid artery. Values are higher in the bulb (1.1mm) and the bifurcation (proximal external carotid artery (0.9mm) than in the common carotid artery (0.7mm)
ariation IMT. Measurements of the intima media thickness in different regions of the carotid artery. Values are higher in the bulb (1.1mm) and the bifurcation (proximal external carotid artery (0.9mm) than in the common carotid artery (0.7mm)
9.8 What are the steps of atherosclerosis?
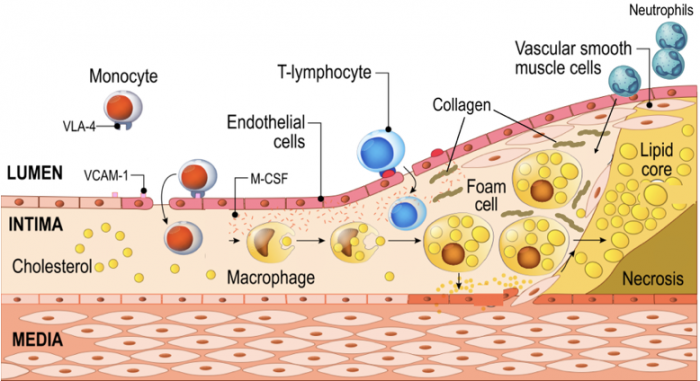 Atherosclerosis. Pathophysiology of atherosclerosis. Endothelial dysfunction is the trigger for a cascade of pathophysiologic events, which eventually lead to plaque formation.
1. Endothelial dysfunction
7. Foam cells promote migration of smooth muscle cells into the intima and media
2. LDL particles enter the intima and get oxidized
8. Proliferation of smooth muscle cells
3. Activation of endothelial receptors for white blood cells
9. Intima - media thickening - plaque formation
4. Monocytes and T-helper cells enter the intima
10. Production of collagen / hardening of plaque
5. Monocytes become macrophages
11. Dead foam cells spill lipid content into the media
6. Macrophages engulf oxidized LDL - become foam cells
12. Further promotion of inflammation (neutrophils)
Atherosclerosis. Pathophysiology of atherosclerosis. Endothelial dysfunction is the trigger for a cascade of pathophysiologic events, which eventually lead to plaque formation.
1. Endothelial dysfunction
7. Foam cells promote migration of smooth muscle cells into the intima and media
2. LDL particles enter the intima and get oxidized
8. Proliferation of smooth muscle cells
3. Activation of endothelial receptors for white blood cells
9. Intima - media thickening - plaque formation
4. Monocytes and T-helper cells enter the intima
10. Production of collagen / hardening of plaque
5. Monocytes become macrophages
11. Dead foam cells spill lipid content into the media
6. Macrophages engulf oxidized LDL - become foam cells
12. Further promotion of inflammation (neutrophils)
9.9 How is the intima media thickness related to plaque formation?
Clearly the larger the intima media thickness is the higher the probability that you will also find plaques. Initially you will frequently find an increase in the echogenicty of the media, sometimes with areas of variable echogenicty (fatty streaks, calcification) followed by an irregular surface of the intima/endothelium. In the later stages you will see build up of plaque.
 MT Irregular Plaque. Increased intima media thickness with an irregular intima surface and beginning plaque formation on the common carotid artery / bulb
MT Irregular Plaque. Increased intima media thickness with an irregular intima surface and beginning plaque formation on the common carotid artery / bulb
9.10 How do you calculate the vascular age of a patient?
The vessel age is calculated using measurements of the intima media thickness of the carotid artery using epidemiologic data. A patient that has a vascular age, which is higher than the chronological age, is at „increased risk“ for cardiovascular events. There are numerous calculators that calculate the vascular age. Some also use other established risk factors for the calculation. Numerous ultrasound scanners already incorporate vascular age calculation into their measurement programs. In essence vascular age is another way to represent cardiovascular risk. While such calculations might help to communicate “risk” to the patient, vascular age has not been widely adopted in clinical practice and vascular age has generally not been endorsed by the international societies.
/* .lity-iframe-container iframe { background: #fff !important; } */ .articles__categories nav { display: none !important; } .sonopl-book__aside .articles__categories { background: #f5f5f5; } .sonopl-article th, .sonopl-article td { color: black; text-align: left; } function advagg_mod_1() { // Count how many times this function is called. advagg_mod_1.count = ++advagg_mod_1.count || 1; try { if (advagg_mod_1.count <= 40) { var getClass = document.querySelectorAll(".articles__categories"); var a = document.createElement('a'); var linkText = document.createTextNode("Get Carotid MC Free Lectures"); a.appendChild(linkText); a.title = "newsletter"; a.href = "/overlay/forms/cu_mc/16618"; a.setAttribute("class", "sonopl-button sonopl-button--default"); a.setAttribute("data-lity", ""); a.style = "line-height: 1.2;margin-top: 25px;padding: 15px;width: 100%;"; for(var ix = 0; ix < getClass.length; ix++) { getClass[ix].appendChild(a) } // Set this to 100 so that this function only runs once. advagg_mod_1.count = 100; } } catch(e) { if (advagg_mod_1.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_1, 250); } } } function advagg_mod_1_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_1(); } else { window.setTimeout(advagg_mod_1_check, 250); } } advagg_mod_1_check(); .pagination .pager .pager__item { font-size: 12px; } .pagination .pager .pager__item--current { padding: initial; } .pagination { margin: 0; margin: 0 auto; margin-top: 0 !important; } .pager { margin-top: 0 !important; padding: 0; display: flex; } .pagination .pager { padding: 0; } .pagination .pager a { padding: 8px 12px; } .pager__item a { box-shadow: none !important; } .aut-nav-carotid-p { text-align: center !important; margin-bottom: 6px !important; } function advagg_mod_2() { // Count how many times this function is called. advagg_mod_2.count = ++advagg_mod_2.count || 1; try { if (advagg_mod_2.count <= 40) { var autNaviCarotid1 = ('\ \
- \
- \
Chapters\
\
- \ 1\ \
- \ 2\ \
- \ 3\ \
- \ 4\ \
- \ 5\ \
- \ 6\ \
- \ 7\ \
- \ 8\ \
- \ 9\ \
- \ 10\ \
- \ 11\ \
- \ 12\ \
- \ 13\ \
- \ 14\ \
- \ 15\ \
- \ last »\ \ \ \ '); var autNaviCarotid2 = ('\
Carotid Ultrasound Webbook & Wiki\ \
- \
- \
‹ previous\
\
- \ BACK TO OVERVIEW\ \
- \ next ›\ \ \ \ '); (function($) { $(document).ready(function(){ $(".sonopl-article.sonopl-book__content.sonopl-content-main") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); $(".aut-nav-carotid") .prepend(autNaviCarotid1) .prepend(autNaviCarotid2); }); }(jQuery)); // Set this to 100 so that this function only runs once. advagg_mod_2.count = 100; } } catch(e) { if (advagg_mod_2.count >= 40) { // Throw the exception if this still fails after running 40 times. throw e; } else { // Try again in 250 ms. window.setTimeout(advagg_mod_2, 250); } } } function advagg_mod_2_check() { if (window.jQuery && window.Drupal && window.Drupal.settings) { advagg_mod_2(); } else { window.setTimeout(advagg_mod_2_check, 250); } } advagg_mod_2_check();
If you like the way we teach, please leave a message!
- \ BACK TO OVERVIEW\ \
- \ 1\ \