10. Atherosclerotic Plaque

10.1 What is an atherosclerotic plaque?
A plaque is a regional thickening of the vessel wall caused by atherosclerosis. Plaques are covered by a fibrous cap and consist of LDL-cholesterol, collagen, smooth muscle cells collagen calcium and different cells (monocytes/macrophages, T lymphocytes, neutrophils and foam cells). Plaque can cause narrowing and occlusion of arteries. Carotid ultrasound allows us to detect and classify plaques (i.e. stable vs. instable, soft vs hard) and thereby assess cardiovascular risk. Plaque formation usually starts with fatty streaks and intima media thickening, which eventually leads to focal wall thickening with progressive narrowing of the artery (stenosis).
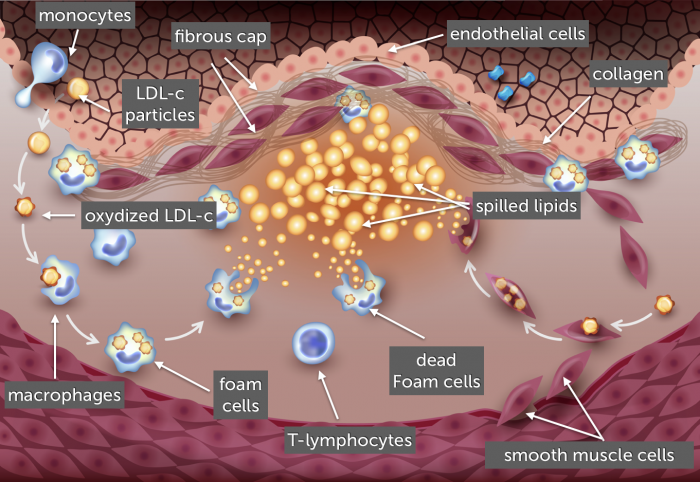
Note: Many atherosclerotic risk factors (hypertension, hyperlipidemia, diabetes) cause damage and dysfunction to the endothelium. This leads to expression of cell adhesion molecules, which allows leucocytes to enter the endothelium (pro-inflamatory effect).
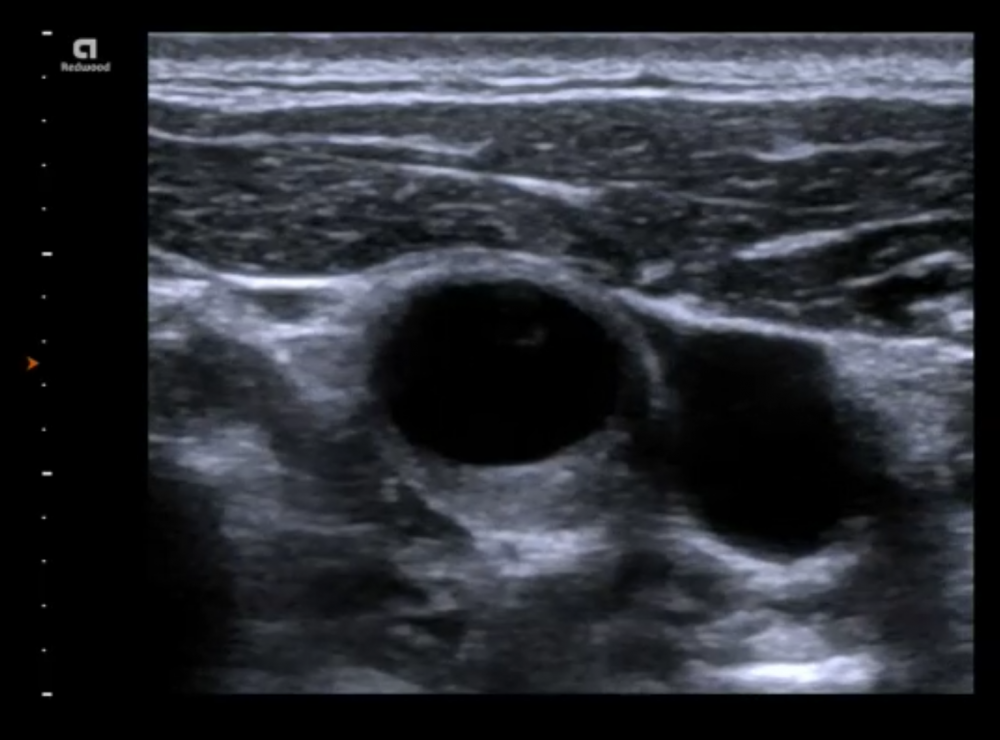
10.2 How is a plaque defined in ultrasound?
The ASE (guidelines) and the European Manheim consensus defined plaques as “a focal wall thickening” measuring either 1,5 mm from the normal reference intima or a focal thickening that measures 50% more than the surrounding intima media complex.

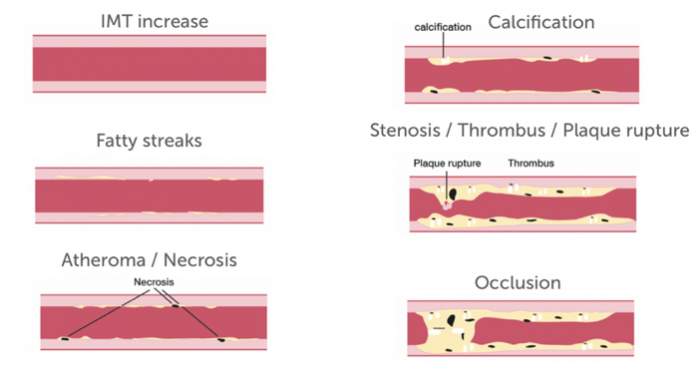
10.3 What are the different stages of plaque formation?
| 1. Increase in IMT | Often combined with an increase in echogenicity of the media |
| 2. Fatty streaks | Inhomogeneous appearance of the IM |
| 3. Atheroma and necrosis | Irregular (non-smooth) IM + echogenic (fibrosis) and echo lucent areas (necrosis) |
| 4. Calcification | Appearance of high echogenic areas (calcification) of variable degree |
| 5. Stenosis | Protrusion of the plaque into the lumen causing stenosis (various plaque morphologies possible |
| 6. Occlusion | No lumen present |
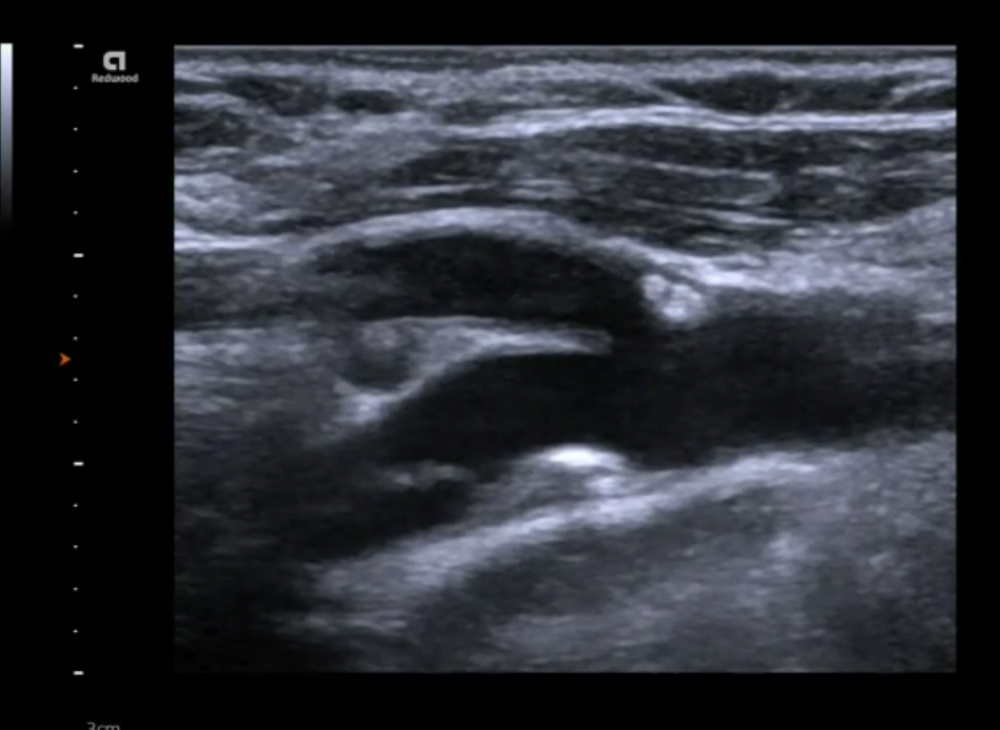
10.4 How do you characterize a plaque?
It is important to classify, describe and provide measurements of a plaque in your ultrasound report. This will allow you to assess the risk of the patient and to determine if a plaque grows over time. Plaque characterization is important to guide patients towards risk reduction and to optimize medical treatment. Plaque morphology is equally important for the surgeon and the interventionalist if endarterectomy or stenting is considered. Here are the different plaque characteristics that should assess and describe in your report:
| Finding | Description |
|---|---|
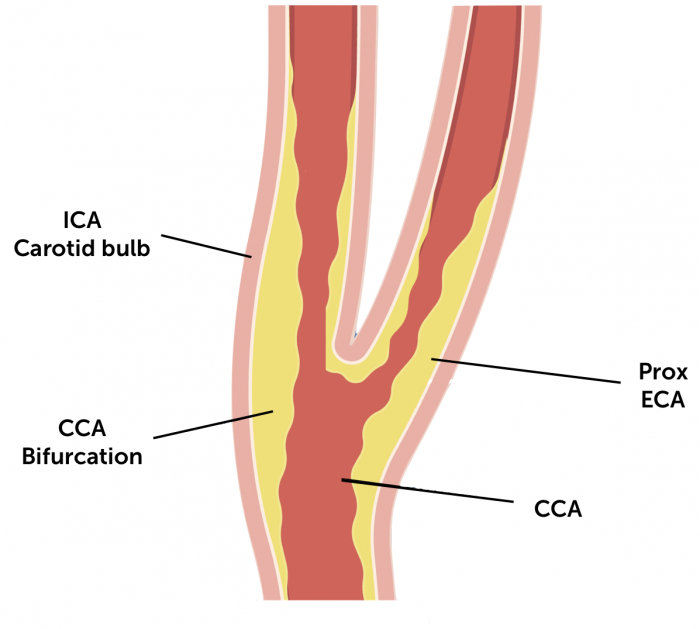
| Location | CCA/Bifurcation/ICA/ECA |
| Wall | Ant/post/med/lat |
| Extent | Length / width / shape (circular eccentric) |
| Echogenicity | Anechoic / isoechoic / hypoechoic /hyperechoic |
| Texture | Homogenous /heterogeneous |
| Surface | Regular / irregular / ulcerative |
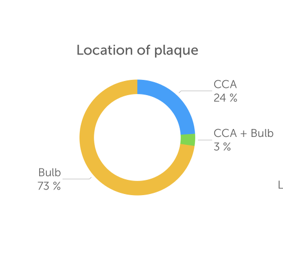
10.5 Where are plaques most commonly located?
Plaques generally form at regions where local hemodynamic forces such as tensile stress (outward deforming force) and shear stress (friction/ force parallel to the vessel wall) are high. In the carotid artery this is the case in the region of the bifurcation and especially in the region of the bulb.
Note: This does not mean you should not image the more distal segments of the carotid artery!

10.6 What does the presence of a plaque in the carotid artery tell you?
Patients with plaque (and stenosis) are at increased risk of stroke and cerebrovascular infarcts. Patients with a high plaque score (severe plaques) have a 10 fold increased risk for lacunar infarctions. Plaques can be the source of an embolus but also a marker of generalized atherosclerosis. Therefore carotid plaques are also associated with the presence of coronary artery disease, peripheral vascular disease and chronic kidney disease. Carotid ultrasound can be used to assess patients with suspected coronary artery disease to determine the likelihood for atherosclerotic disease.
10.7 What is a vulnerable, high-risk plaque?
Some plaques are at increased risk of plaque rupture, thrombosis and rapid progression. Much of the knowledge we have about vulnerability of plaques has actually been obtained from studies of coronary artery plaques. We now know that several factors such as active inflammation (macrophage-mediated), neo-vascularization (vessels growing into the plaque) and hemorrhage as well as hypoxia, and micro-calcification predispose to instability. While ultrasound does not provide histological information, we can obtain clues that point to higher versus lower stroke risk. The following characteristics are associated with the vulnerability of plaque:
- Larger thicker plaques (>1cm in length, plaque diameter >4mm)
- Number of plaques
- Rapid progression of plaque
- Echolucent plaques (lipid rich soft plaque)
- High plaque score (score based on the degree of stenosis the surface characteristics and echogenicity)
- Irregular surface
- Eccentric plaque
- Mobile structures / thrombus
- Ulcerations, intraplaque hemorrhage, necrotic core (echolucent areas within a plaque)
- Neo-vacularisation (contrast / color Doppler flow within a plaque)
- Problem: Most criteria are subjective - operator dependant
10.8 What is neo-vascularization of a plaque and how can it be detected with ultrasound?
Vasa vasorum (small vessels in the adventitia that supply the artery wall) can proliferate (angiogenesis) and grow into a plaque. The trigger for neo-vascularization is probably hypoxia, which occurs when the vessel thickens. Neo-vascularization is associated with intra-plaque hemorrhage and therefore contributes to plaque instability. Contrast enhanced ultrasound can be used to detect neo-vascularization. Using contrast ultrasound one can see the micro-bubbles of the contrast agent (blood flow) within the plaque.
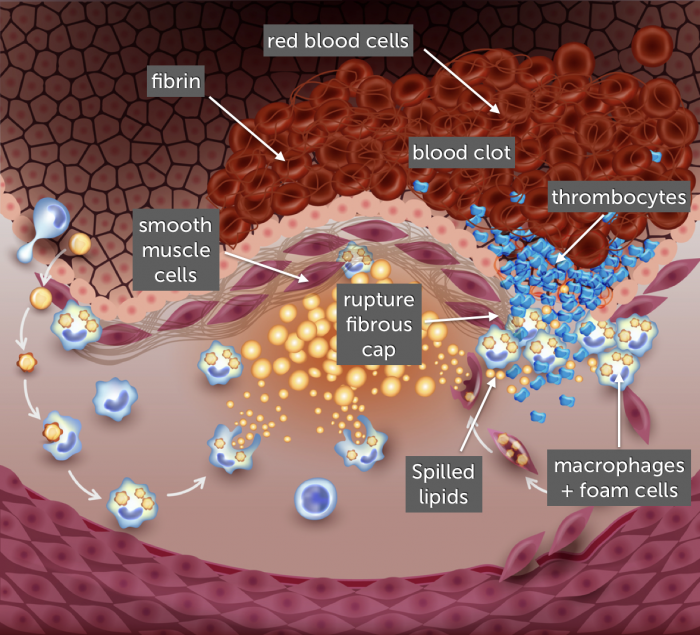
10.9 What is plaque rupture?
An atheroscerotic plaques are covered by a fibrous lipid cap. Tension on this fibrous cap (tensile and shear stress) and/or instability within the plaque (i.e. inflammation, necrosis) can lead to rupture of the fibrous cap and plaque rupture. Lipid rich plaques with a thin cap with little collagen content are at increased risk. Rupture of a plaque leads to exposure of the thrombogenic core to the blood stream. This causes thrombus formation with the risk of:
- Vessel occlusion
- Embolization of thrombotic material.
Ruptured plaques can also heal. This process contributes to plaque growth calcification and plaque fibrosis.
Note: The risk of plaque rupture is related more to plaque morphology and composition than to plaque size or the degree of stenosis.
If you like the way we teach, please leave a message!