Second Look

We are all influenced by the law of probability. Hoofbeats are more likely caused by a horse than a zebra, a loud crash is more likely a car accident than a meteorite plunging into Earth, and the sudden pain you feel when you are in the swamps will most likely be an insect and not the poisoned dart of a tribesman at war.
But probability also means that the unlikely may occur at times. The following case illustrates this concept.
Tirana meets Vienna
Arita, a 45-year-old woman from Tirana, Albania, had fever, dyspnea and swollen ankles for some time. She went to several doctors in her country, who told her that she had a serious “heart” condition which needed cardiovascular surgery. Seeking a second opinion, she eventually came to Austria. At the time her CRP levels were slightly elevated, she had thrombocytopenia, and she complained of fatigue. Her BNP levels were also slightly elevated (534 pg/ml).
Putting two and two together
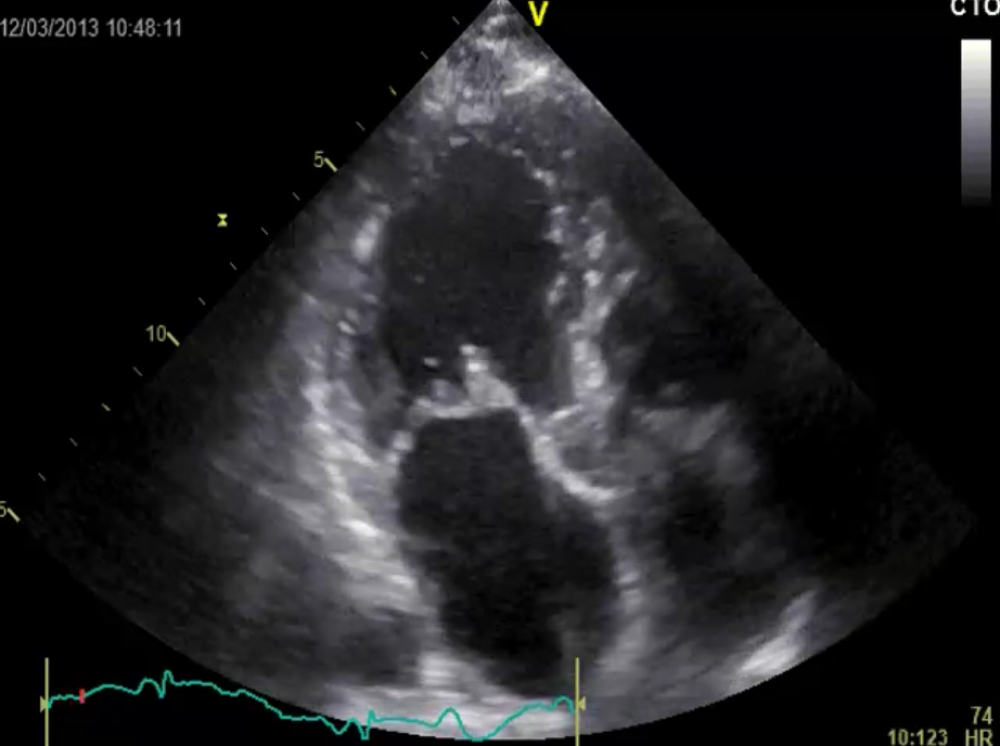
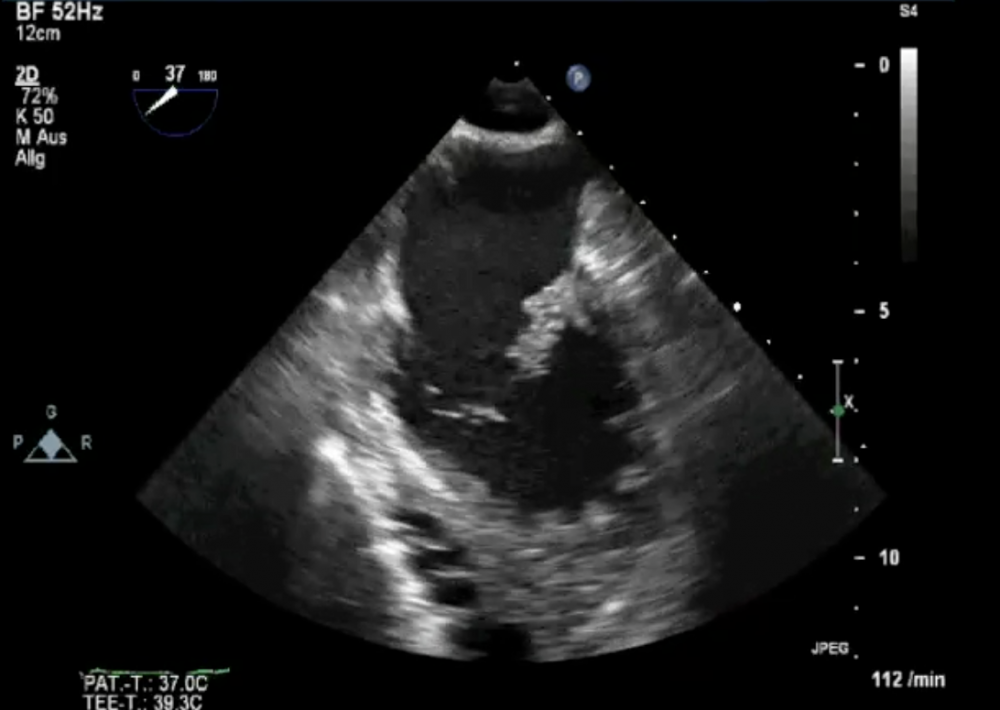
This was the echo that I performed at the time:
Sure enough, her mitral valve was thickened and there were small vegetations attached to the valve.
So the diagnosis is quite clear: infection + vegetations = infective endocarditis.
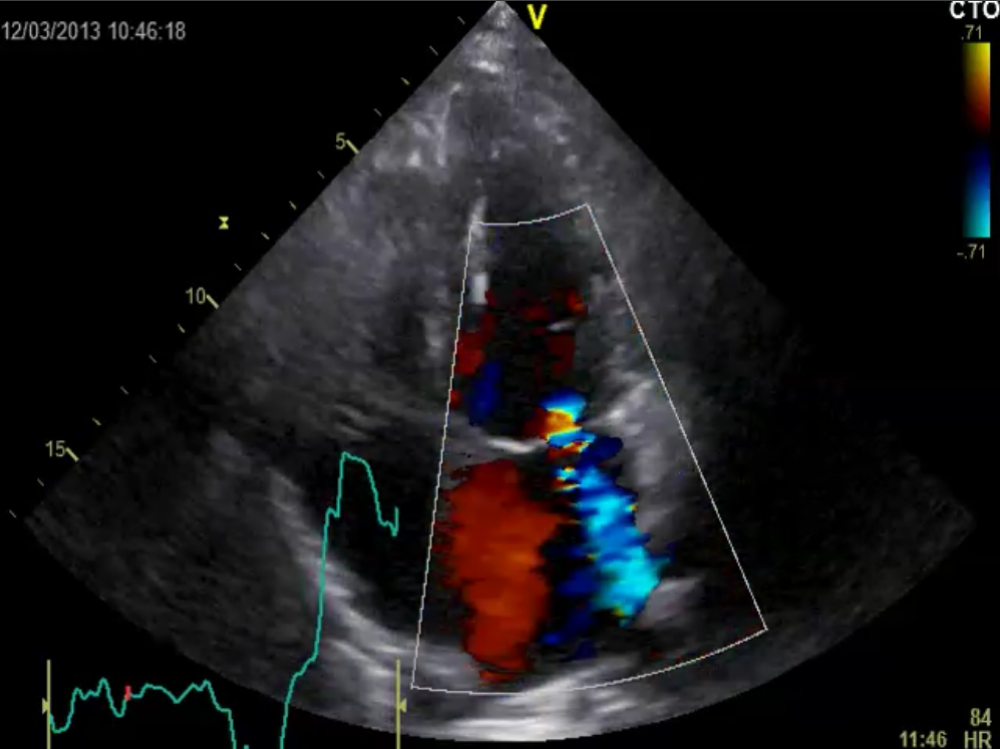
Clearly, there is at least moderate mitral regurgitation. The infection was destroying the valve.
A crystal clear diagnosis
I wasn’t sure whether all of the structures dangling around the valve were really vegetations, or whether there was destructive leaflet tissue as well. After all, her problems had started several months ago. With active infection on the valve for such a long time, the valve was probably melting away. Since she was rather stable the vegetations did not seem to bear a high risk of embolization. Hence we decided not to operate at that time. Blood cultures proved to be negative, so we gave her a high dose of a standard regimen of antibiotics, which kills practically any bacteria one can think of. She actually improved.
A second look
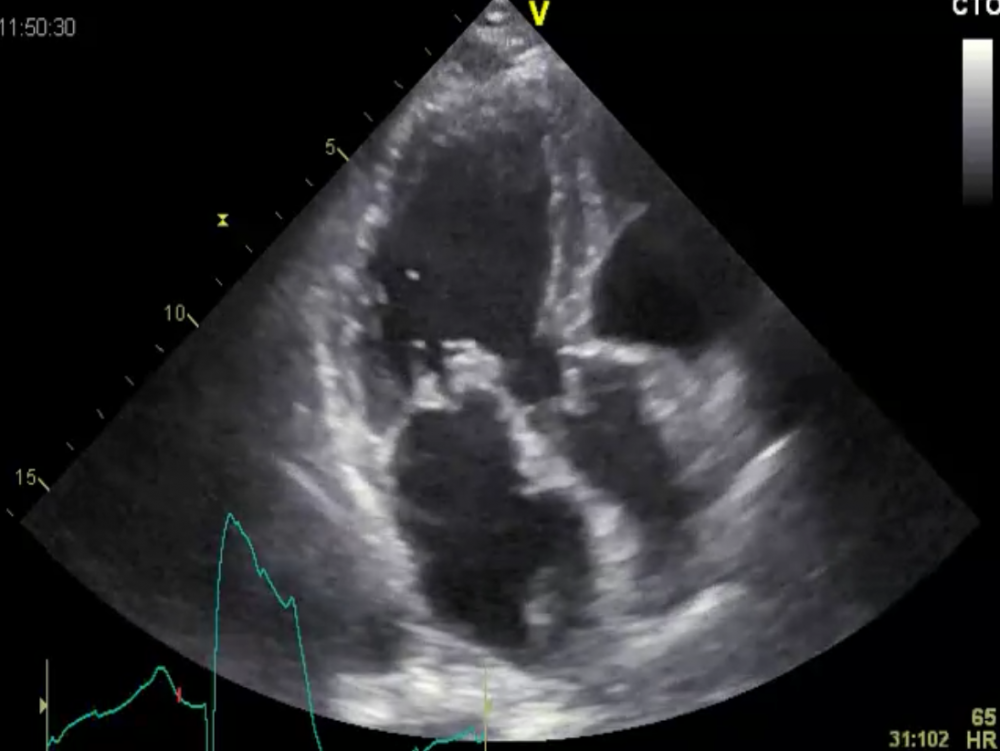
I lost track of Arita, but I heard she had returned to Albania. She came back after a year. Her dyspnea had improved, but she was now suffering from general fatigue. Before she came her treating physician (a friend of mine and a really smart doctor) performed an extensive work-up that put her echocardiographic findings into a new perspective. However, before I let you read her new diagnosis, let me show you the follow-up echo.
At first glance her mitral valve looks quite similar to the first study. But if you look more closely, you will note that the findings are even more prominent now. Is this a slow progressive form of infectious endocarditis? Was the antibiotic treatment ineffective?
The valve (including the subvalvular apparatus) is severely thickened and the vegetations seem to be larger. What about valve function?
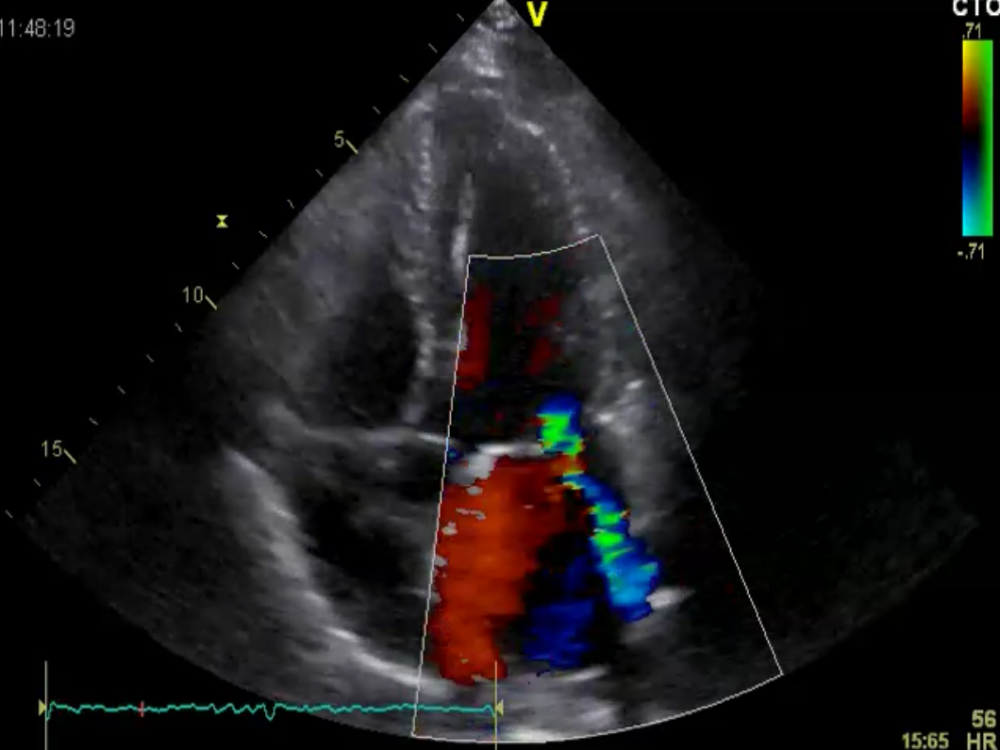
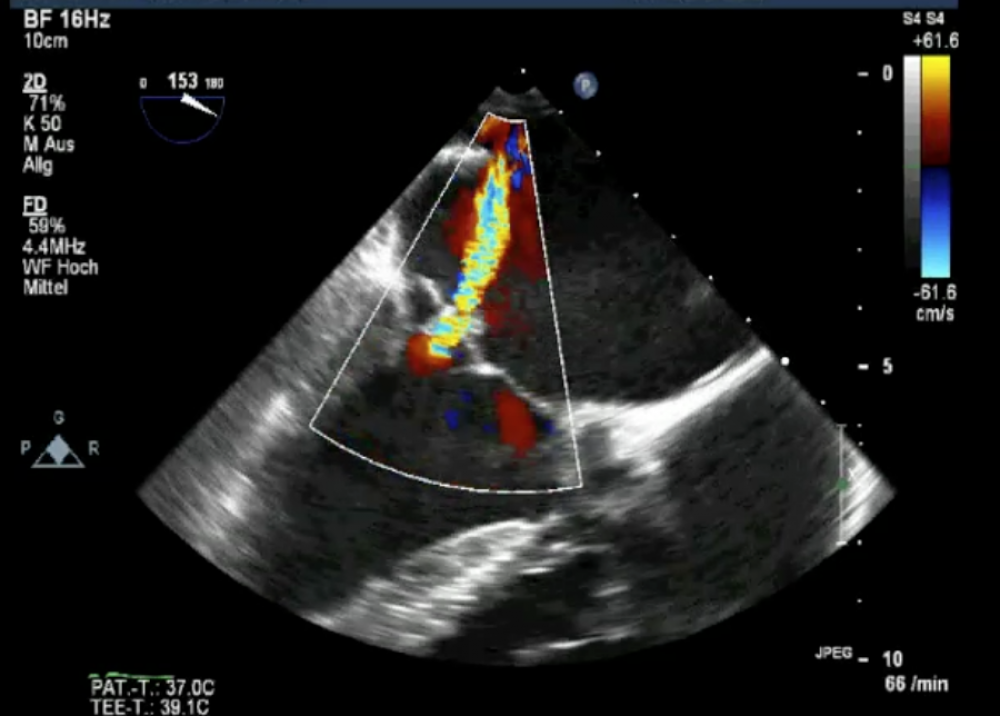
Her mitral regurgitation also worsened slightly. It is not severe yet, but the progression of MR also points to a chronic valvular problem (or additional annular dilatation).
At the time of this study I had been informed that Arita had an autoimmune disorder. Most likely systemic lupus erythematosus (SLE) or some closely related variant, but one thing was clear: her antiphospholipid and cardiolipin antibodies were high.
Zebras and not horses
How does this change the probability?
What does her valve pathology make you think of in terms of diagnosis?
Yes, Libman-Sacks endocarditis in the setting of antiphipholipid syndrome. This was the explanation for the thickened valve, the vegetations, and her general condition. It also explains her thrombocytopenia.
About 1 in 10 patients with SLE will have this form of endocarditis. The vegetations are accumulations of immune complexes and mononuclear cells, and can be seen on the atrial AND the ventricular side of the valve. The vegetations are prone to the risk of embolization. The degree of involvement is closely linked to the patient's antiphospholipid and cardiolipin titers.
Here is her follow up TEE, showing the full extent of the problem.
The vegetations resemble mulberry-like clusters of verrucae. While significant regurgitation is rather uncommon, Arita does have MR. I am afraid this will eventually cause a problem.
The degree of regurgitation can best be appreciated on this view. I presume the autoimmune infection causes some form of valve damage.
The full extent of valve involvement can be seen on the 3D echo image.
Note that large portions of the anterior leaflet are covered with a thick layer of vegetation.
A word from Dr. House
What are the key messages here? First, as Dr. House says, always consider SLE as a differential diagnosis. Second, obtain more information about patients before jumping to conclusions. Probabilities may change quite significantly when you know more about a case. After all, zebras are more common than horses in Africa.
What about Arita? She is now under treatment with corticosteroids and anticoagulation therapy. Let's hope her SLE can be controlled and her valve does not worsen. Valve surgery in the presence of lupus can be quite problematic, as the repaired or replaced valve may also be affected by the immune disease.
PS: If you like this Newsletter please forward it to friends who might be interested.