One heart, too many emotions…the sequel!

Do you remember dear Paul, the young Viennese engineer who stabbed his heart? Urgent surgery to stitch up his right ventricle certainly saved his life - but he still had a large VSD.
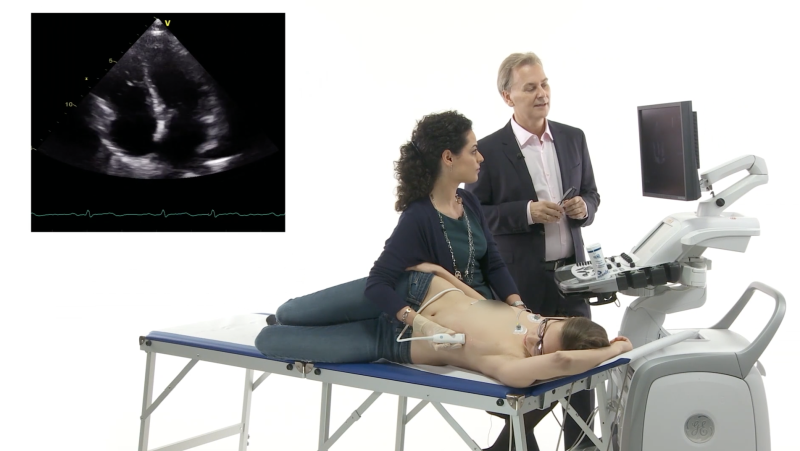
Apical four-chamber view with color Doppler
showing a huge left-to-right shunt.
We named the case story “One heart, too many emotions”. Many of our users were curious to know how things evolved after the diagnosis had been established. Well, here is the sequel, which will show you a novel approach for the treatment of patients with a ventricular septal defect.
Decision-making
Our discussion focused on several issues: Paul was still alive, but he had lost a lot of blood; he was hemodynamic unstable. We could not neglect the risks of surgery. How urgent did we have to intervene? His ventricle was starting to adapt to the volume overload but the VSD had to be closed in order to avoid irreversible damage to the heart (LV dilatation, increase in pulmonary vascular resistance). How should it be closed? Was surgery the only option? Muscular VSD´s can be treated percutaneously; the important thing is to select the right device. Moreover, Paul’s defect was very close to the moderator band and papillary muscles: conditions that surgeons do not like. After a session of brainstorming, we opted for the percutaneous approach. Harald Gabriel and Günter Stix, our interventionist, were eager to solve the problem.
Elective minimally invasive catheter procedure
Paul looked different when he was re-admitted to the hospital. After receiving appropriate psychological and social support he was self-confident and strong. The intervention was performed under deep sedation, with fluoroscopic and echocardiographic guidance (transthoracic echocardiography, TTE).
The procedure step-by-step
The right femoral vein and artery were punctured. A complete hemodynamic evaluation with oximetry and pressure measurements was performed. The size of the defect was assessed with TTE and ventriculography. The device shown below was chosen to close the rather large defect.
 Device: 20 mm Muscular VSD AMPLATZER P.I. Occluder.
Device: 20 mm Muscular VSD AMPLATZER P.I. Occluder.
An arterial-venous loop was then created (a catheter was passed into the right femoral artery and was gradually advanced through the aortic valve, the VSD, the right ventricle and the tricuspid valve. It was then drawn into the inferior vena cava and out from the right femoral vein, as shown below).
(created by passing the guidewire through the VSD).
A delivery system was advanced from the venous side through the defect into the left ventricle. The device was then introduced for deployment.
Look below at the fluoroscopic (left) and TTE (right) loops: the first disc was released and opened into the left ventricle. It was then pulled back to adhere to the interventricular septum. This step of the procedure required TTE in order to confirm the correct position of the first disc (left ventricular side).
The following two loops show the release of the second disc (right ventricular side).
(left: fluoroscopy, right: echo).
Final outcome
Once the device was correctly placed, the delivery system was detached and a final functional assessment was performed using fluoroscopy and echo.
A residual small left-to-right shunt was detected. There is a high likelihood of the shunt gets even less once by endothelialization of the device occurs.
showing the device and the residual shunt.
Wrapping up the case:
Paul was really glad everything went so smoothly. And so were we. Not only because we could help him, but because Paul regained his will to live.



 Anna Maria Pistritto, Harald Gabriel, Günter Stix & Thomas Binder
Anna Maria Pistritto, Harald Gabriel, Günter Stix & Thomas Binder
PS: We are curious to hear your comments: So don’t forget to post them here.
PPS: Don’t forget to catch up on some of the latest cases we posted. We have lots of interesting free stuff on our blog.