Outside the box

Or daily routine often forces us to stay focused and only do to what we are told to do. Not to look left or right. But this also means we are deprived of making important discoveries that might impact our patients. Here is such a case:
A 59-year-old patient was referred for echo after an inferior myocardial infarction, two-vessel stenting, and exertional dyspnea.
The images below clearly show that he has a scar in the inferior region and that his left ventricular function is somewhat reduced.
Apical view showing a scar in the basal septum, extending inferior. Left ventricular function is mildly decreased
Should we stop here?
No! There is much more than ultrasound has to offer: Let us now take a linear transducer and move more lateral to the base of the lungs to find out if our patient has pulmonic congestion?
Lung ultrasound shows 1 or two B-lines. This is not enough to call this congestion
While there are a few B-lines, lung ultrasound helps us to exclude that the patient has heart failure - an important piece of information that will help us guide therapy.
We are not done yet
Especially in patients with vascular disease we have to gather as much information as possible to assess risk and optimize secondary prevention. Wouldn’t it be interesting to know if our patient also has carotid artery disease - if he is also at risk of stroke?
After all we know that carotid artery stenosis (>50%) is present in 25% of patients with coronary artery disease.
And here is his carotid artery scan:
A few echogenic (hard) plaque seen in the bifurcation. Note that the bifurcation is also a bit dilated
We see plaque in the region of the bifurcation but - thank god - no stenosis (normal flow velocity in the internal carotid artery).
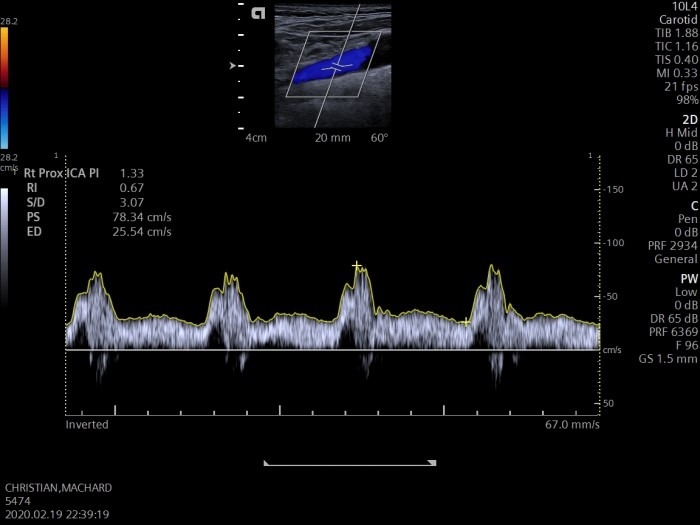
Spectral Doppler study: normal flow velocity in the proximal internal carotid artery. No stenosis is present
From head to toe:
While scanning the patient told me that he occasionally feels numbness in his left toes. Not expecting to find much I scanned his peripheral arteries.
What a surprise!
Take a look at his left popliteal artery!
Scan of the popliteal artery demonstrating a large (3.5cm) aneurysm with layers of thrombotic material, but no obstruction
Color Doppler scan of the popliteal artery in a short axis: Popliteal aneurysm with circumferential thrombus and a residual lumen (no obstruction)
A huge aneurysm measuring 3.5cm in diameter, filled with clot! This diagnosis definitely makes a difference!
Popliteal aneurysms are not as uncommon as it may seem. The popliteal is the second most common location for aneurysms following aortic aneurysms. In 10% of patients with aortic aneurysms, you will also find popliteal artery aneurysms.
What this means
A Popliteal artery aneurysm is not a benign condition. Not only because it can rupture (2-7%) but what is even more important because it can lead to limb ischemia (50%) and might require amputation.
Of course, our patient was not happy about the diagnosis. But never the less he was very thankful. He will now undergo surgery.
The bottom line.
The more you look the more you will find. Most of the time you will not need supernatural powers to make a difference. All you might need is that little extra effort and a breeze of curiosity.
Best Thomas Binder and the 123sonography team





