Fear of Complexity
Complexity scares us. It tends to defy our comprehension skills. However, we sometimes make things more complex than they actually are. Two such subjects are tamponade and pericardial constriction. True, understanding the physiology of constriction involves a lot of thinking. Pericardial and intrathoracic pressures, interventricular dependence of the ventricles, respiratory variations - all of these factors play a role in what you see on the echo. Let me put it this way: do we really have to understand all these aspects in order to make a diagnosis? Can't we just look for a few typical features, combine them with the patient's clinical appearance, and establish the correct diagnosis?
I think one can, and I assure you - once you have seen a few cases you will also start to understand the physiology behind your findings.
A typical case
Here's a typical case: A 55-year-old woman presented with shortness of breath, a history of fever, as well as peripheral edema and hypotension. Sure, her condition could have been anything from endocarditis to myocarditis, or simple heart failure. But once you look at the echo you realize that several things are very unlikely while others are just waiting to be detected.
The septal shift
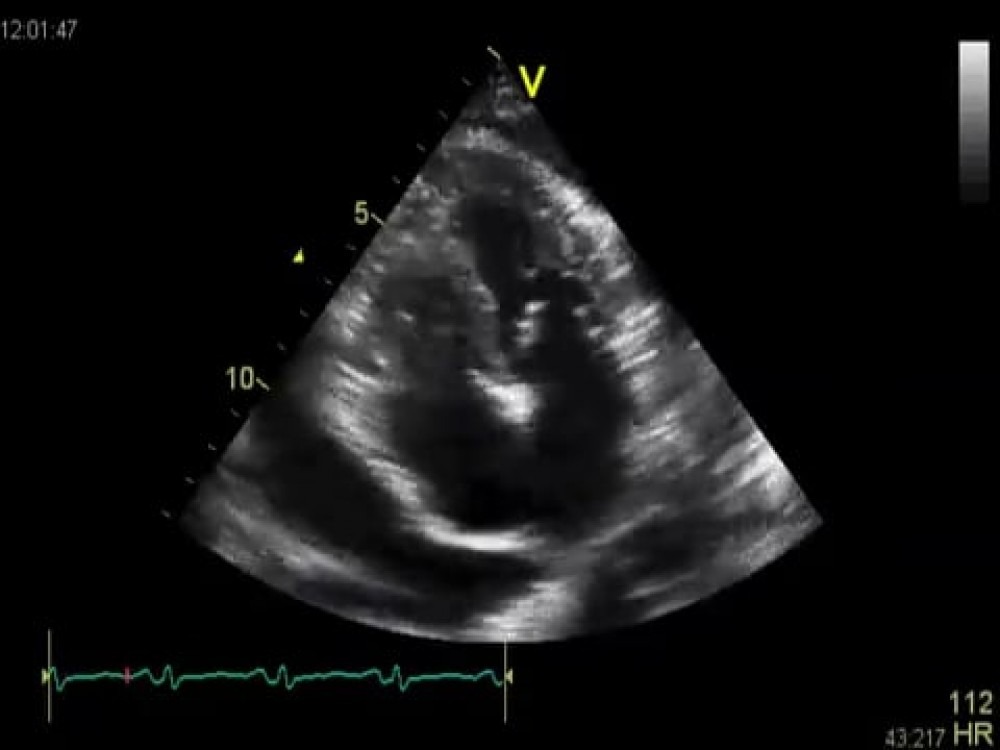
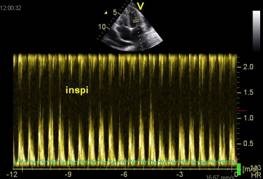
Look at the following four-chamber view:
It is not difficult to see the pericardial effusion - an important finding, as you will see later. Do you think this patient has dilated cardiomyopathy? Certainly not, because the left ventricle is normal in size and systolic function is normal as well. Still, there is something awkward about the way the ventricle contracts. Look at septal motion. The loop was recorded exactly when the patient inhaled. Can you see how the septum wiggles back and forth and suddenly shifts to the left?
In my mind, this is the most important feature when you are looking for a tamponade or constriction. We are on the right track. Let us now confirm what we saw on the subcostal view:
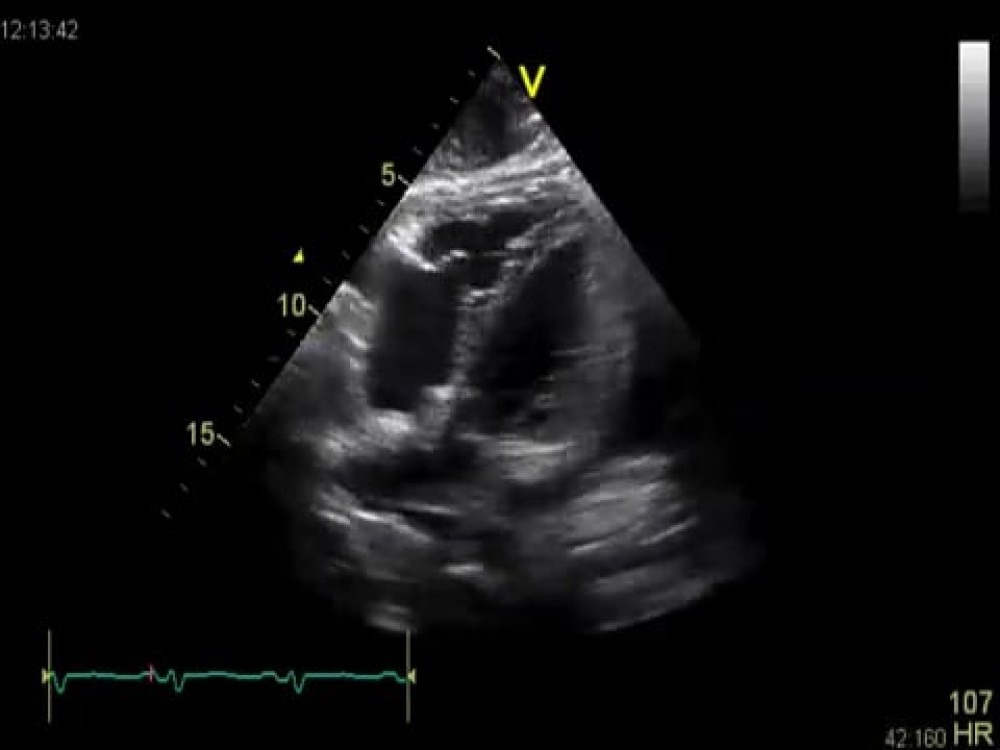
“Sticky pericardium”
The pericardial effusion seems to be very “organized” and fibrous here.
What does this tell you? That it is probably the result of a bacterial infection. An important finding! Take a close look at the motion of the pericardium here. It appears to be dragged inward during right ventricular contraction - as if it were stuck to the heart. This view also shows the “septal shift” which we saw on the four-chamber view. Moving the transducer to the right reveals the inferior vena cava.
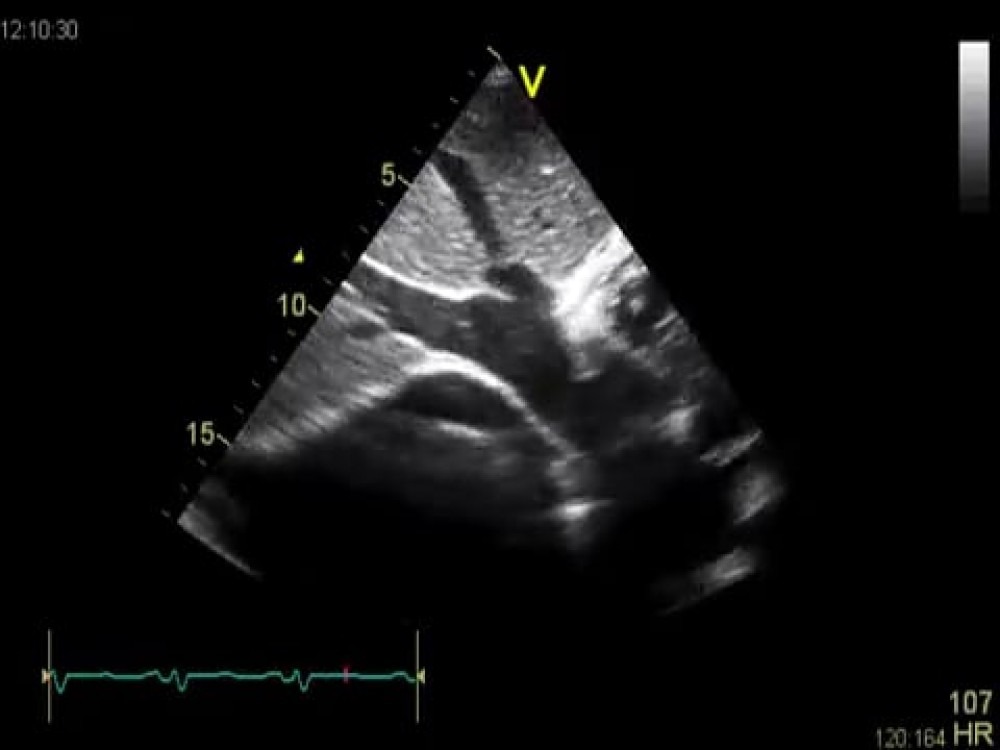
Venous congestion
What happens when you constrict the heart? It will not be filled easily. Blood will collect in the vessels leading to the heart. This is exactly what you see here:
Both the inferior vena cava and the hepatic veins are significantly dilated. This condition MUST be present when you have symptomatic pericardial constriction - just as pleural effusion, hepatomegaly, jugular venous distension, and peripheral edema are hallmarks of the disease. Pericardial effusion is also seen in this view.
But couldn’t it also be restrictive cardiomyopathy?
Many features of restrictive cardiomyopathy are similar to those of pericardial constriction. These patients may present with the same clinical features as those described above, but hepatic venous flow looks different in these patients. Why am I not showing you this signal? To make things more simple. The hepatic venous signal is not only difficult to obtain but quite inconclusive and very difficult to interpret. This is what I would recommend:
Keep it simple
First, look at the atria: they are normal in size. You will rarely see this in restrictive cardiomyopathy. Next, obtain a pulsed-wave Doppler signal of transmitral flow and set the sweep speed to the lowest possible velocity.
Look at the fluctuations of E-wave velocity, especially the decrease of velocity in response to inspiration. What you see here is impaired left ventricular filling caused by constriction, which is more prominent during inspiration. Fluctuations of inflow velocity are caused by the same phenomena that cause the septal shift. The right ventricle fills more during inspiration. Normally the left ventricle is not affected, but if it cannot expand as in constriction, the septum shifts to the left. The ventricle becomes smaller and is less easily filled.
Make it even more simple
For all of you who have tissue Doppler (TDI) on their machines, there is another easy trick you can use:
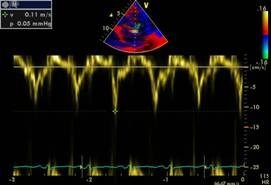
Measure the E´ velocity in such patients. In pericardial constriction, it will be fairly high (> 0.08 m/s) while it will be very low in patients with restrictive cardiomyopathy (< 0.05 m/s).
Viewing all this in a clinical context
As it turned out, our patient had tuberculosis - a common cause of constrictive pericarditis, especially in developing countries. Since pericardial effusion is also present, one should correctly refer to the condition as “effusive-constrictive pericarditis”. In such cases, constriction is present even after intrapericardial fluid has been removed. One has to wait and see whether fixed constriction persists after the infection has been controlled. Signs and hemodynamics, however, are the same as those in pericardial constriction.
It's not very complex - all you need is a suspicious mind and good scanning skills to look for key findings.
What's next?
Do you want to become a true echo expert, a respected authority in your hospital? Someone that others rely on and look up to? Yes? Well, then you should definitely check out our Masterclass. There, you'll learn everything you need to know in order to examine over 95% of your patients without the help of someone who is more senior than you. Learn this powerful tool and make better clinical decisions!