One heart, too many emotions
“Feelings are so difficult to deal with. Sometimes they make you so excited and joyful that you can almost touch heaven. At other times they force you on your knees and you forget how to get back on your feet.”
This is what our patient, Paul, a 36-year old engineer from Vienna, told us five days after surgery.
Prologue
One day, without any forewarning, Paul’s landlord asked him to move out. Lawyers were called from both sides and periodic fights became a routine occurrence from then on. Anger, confusion and discouragement tormented Paul. With each passing day he became more and more fragile. Soon the entire situation became unbearable. Early one morning, Paul grabbed a knife and stabbed his heart.
The run to the hospital
As the door of the flat was open, Paul’s neighbor saw him and immediately called 9-1-1. Paul was wheeled into the operating room right away. The knife was still in place, preventing any massive flow of blood from of the right ventricle.
Back to life but...
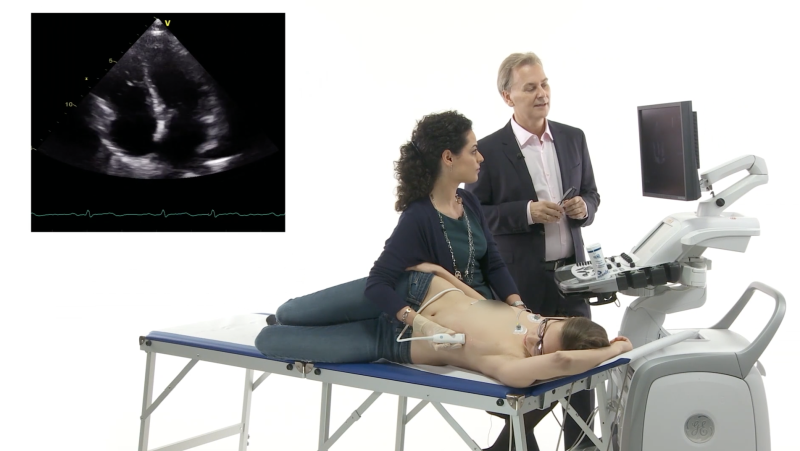
After the right ventricle had been sutured and the chest closed, Paul was sent to the intensive care unit. The first postoperative transthoracic echo (TTE) showed that the nightmare was not over yet. Look at Paul’s heart and establish the diagnosis yourself.
Parasternal short-axis view – hyperdynamic function
Apical four-chamber view: hyperdynamic left ventricular
function; the ventricle is very slightly dilated.
.
Paul’s heart was working hard! Both ventricles were of normal size but their function looked “super-normal”. Have you found out why? Not difficult to diagnose, especially if you add color Doppler to the same views.
Parasternal short-axis view – color jet passing
through the interventricular septum
Apical four-chamber view: you see it clearly here -
a big ventricular septal defect (VSD).
VSD and pulmonary hyperflow
A huge VSD with a massive left-to-right shunt was diagnosed. This meant relevant pulmonary hyperflow. Systolic pulmonary artery pressure (sPAP) was around 80 mmHg.

Continuous-wave Doppler across the tricuspid valve.
The peak velocity of the tricuspid regurgitant jet is around 4 m/s.
Congenital or acquired VSD?
Considering Paul’s history, of course, we thought about an acquired defect (the knife had gone too deep into the heart). Actually this VSD looked different from a congenital one. First of all it was located at an unusual site - right in the middle of the muscular part of the interventricular septum. Congenital VSDs are usually perimembranous (around 80% of them). Secondly, the left ventricle was not dilated, which meant it had been dealing with this blood volume overload for a rather short period of time. Thirdly, such a big VSD would have evolved easily into Eisenmenger syndrome (right-to-left or at least a bilateral shunt with a hypertrophic dilated right ventricle and increased pulmonary vascular resistance) if it had been present since birth. Here the shunt is exclusively left to right.
Hemodynamic consequences
How is Paul’s heart reacting to this new hemodynamic condition? His heart rate (HR) as well as his stroke volume (SV) have increased in order to sustain his cardiac output (Q).
However, because of the same left-to-right shunt, the quantity of blood crossing the pulmonary valve at each systole and entering the pulmonary circulation is greater than the quantity of blood crossing the aortic valve to enter the systemic circulation. In other words, right ventricular SV is higher than left ventricular SV. Obviously, the same is true of his cardiac output: pulmonary Q > systemic Q (Qp>Qs). The Qp/Qs ratio can be assessed by echo. It is the principal way of quantifying the degree of a shunt across a defect. It also provides precise indications as to whether and when the defect should be closed. Do you want to know how to calculate Paul’s Qp/Qs? Read Box 1 for the details.
We know that Q = HR x SV. Paul’s HR is 93 beats/minute, so all we need to do is calculate right ventricular SV (SVp) and left ventricular SV (SVs) in order to obtain Qp and Qs, respectively.
Qp = HR x SVp; Qs = HR x SVs.
SVp can be calculated by measuring the cross-sectional area of the right ventricular outflow tract (RVOT) and the quantity of blood flowing through this area. The latter is expressed as the VTI (velocity time integral) of flow across the RVOT*.
SVp = RVOT area x RVOT VTI = π (RVOT diameter/2)2 x RVOT VTI
VTI is expressed in centimeters and obtained by placing the pulsed-wave Doppler in the RVOT and tracing the signal’s envelope, as shown below.

Pulsed-wave Doppler in the right ventricular outflow tract (RVOT), showing a high VTI (25.1 cm).
The same formula can be used to assess SVs by taking the left ventricular outflow tract (LVOT) area and VTI into account:
SVs = LVOT area x LVOT VTI = π (LVOT diameter/2)2 x LVOT VTI.
As you can see from the figure below, LVOT VTI was much less than RVOT VTI.

Pulsed-wave Doppler on the left ventricular outflow tract (LVOT).
The velocity-time integral (VTI) is only 18.9 cm.
* Alternatively one may use the site of the pulmonary artery to calculate stroke volume.
Decision making
Paul’s Qp/Qs was finally 1.7. Since patients with VSD and pulmonary arterial hypertension (PAH) should be considered for surgery when they still have a clear left-to-right shunt (Qp/Qs >1.5) and their pulmonary artery pressures (PAP) or pulmonary vascular resistance (PVR) are < 2/3 of systemic values, we had no option than to again send Paul to the operating room, hoping for the best.
Key messages
The following are the key aspects of this post:
- how to discern between acquired and congenital VSDs;
- how to interpret relevant changes in cardiac hemodynamics in the presence of acute VSD;
- how to assess pulmonary to systemic flow ratios by echocardiography, and
- what parameters one should take into account (Qp/Qs, PAP and PVR) when considering invasive treatment.
Let us know whether you enjoyed the case… we’ll let you know how it ended.

Anna Maria Pistritto